A Guide To Treating Post-Pill Acne
All products on this page have been selected by our editorial team, however we may make commission on some products.
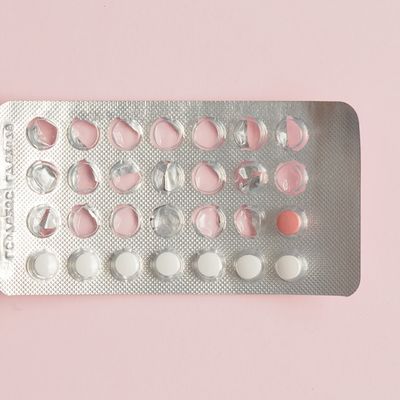
UNDERSTANDING WHAT POST-PILL ACNE IS & COMING OFF IT SAFELY
Why hormones are the culprit…
Post-pill acne often occurs if you take the combined pill, which specifically targets hormonal imbalances and therefore exacerbates acne and breakouts. This is usually because they contain multiple hormones which work to keep your natural hormone levels steady. This in turn can have an adverse effect and make your pores more prone to a build-up of sticky oils, which is called sebum. This can set off a cycle of inflammation and clogged pores that leads to acne and multiple breakouts.
Why it’s not dissimilar from regular acne…
“Post-pill acne can typically flare up for two to six months after you stop taking the pill. The acne lesions can vary from blackheads to whiteheads and even cystic lesions, in the same way that regular acne lesions can present. However, lesions can be both inflammatory and non-inflammatory.”
Why it can affect you at any stage of life…
Whether you're in your early 20s or 30s, have been on the combined pill since your late teens or even if you’re perimenopausal, post-pill acne can be something that affects you. If you’re at a later stage in life, some people experience a ‘reverse puberty’ process, with chaotic hormone products and androgen hormones dominating and switching on the oil producing glands, which is what causes an excess of sebum and therefore acne.
Why it isn't dangerous…
From a skin health perspective, although a post-pill acne flare can be very distressing, the actual process of coming off the pill is not harmful or dangerous, so long as you speak with your doctor first. If you are coming off the pill as a result of skin concerns, the main risk is experiencing an unwanted pregnancy. Therefore, part of the planning process should involve speaking to your physician about alternative contraceptive methods.
Why you should speak to a specialist first…
See a skin specialist who can help prepare your skin in advance of coming off the pill. They can prescribe skincare that will keep the skin calm and breakout free. I recommend allowing a minimum of three months for this. It’s also helpful to have a specialist review your existing skincare products and make-up to ensure you’re not using anything that may trigger breakouts in the future.
KNOWING WHAT TO AVOID
Why taking a break from SPF could help…
While we know how important SPF protection is for the prevention of UV damage and premature ageing, when you’re first starting a post-pill acne regimen, I’d advise pausing the SPF and reintroducing it after a break. Typically, it’s best to wait around six weeks. When the skin is calmer, try introducing a mineral-based SPF, such as zinc oxide or titanium dioxide, which are generally more ‘pore friendly’.
Why choosing non-comedogenic products is key…
The primary form of acne lesion is the comedone, which relates to an area of your skin called the pilosebaceous unit. This is made up of the pores, sebaceous glands (oil producing glands) and hair follicles. When the sebaceous glands get blocked with oil, bacteria and debris, it causes a comedone or spot. Non-comedogenic products are designed to avoid blocking the pilosebaceous units. These tend to be water-based products rather than oil-based ones, as the latter are well known to irritate breakout-prone skin.
Why some skincare and make-up should be avoided…
Skin is likely to react more sensitively once you come off the pill, so product overloading won’t do it any favours. In terms of make-up, concealers, foundations and powders with heavy coverage will also clog up pores. This will then trap oil and bacteria along with dead skin cells and cause pimples and breakouts. Instead, look for mineral based make-up. These products are formulated with finer particles that don’t clog the pores and still offer great coverage. I especially love bareMinerals for this. As for skincare, avoid foaming cleansers, facial oils and mechanical exfoliators.
Why you may want to skip primer too…
If you are prone to oily skin and breakouts, you should also skip primers. They act as an occlusive layer that clogs pores and can lead to dull and lifeless looking skin. Instead, look for replenishing moisturisers that can act as a primer, while keeping your skin in good condition. That’s not to say you must cut it out completely – just save them for a heavier make-up look or special occasion.
Why excessive fake tan isn’t a great idea…
Wearing fake tan can make breakouts worse, but if you do want to use tanning products, apply them in the evening, after cleansing. Leave the product on your face for a few hours and wash it off before bed. Repeat this a few evenings a week. I find this ‘short contact’ tanning process is less aggravating.

FINDING A REMEDY TO TREAT POST-PILL ACNE
Why medication could be worth a try…
There are a whole host of over-the-counter remedies available to address all types of acne, but if the problem is persistent and causing real distress, speak to your GP who may recommend a prescription. Medications such as oral antibiotics, the contraceptive pill or Roaccutane (a vitamin A derivative) may be prescribed for more severe cases.
Why in-clinic treatment might be the only option…
More advanced acne treatments can be found at specialist clinics. Chemical peels, microdermabrasion and laser treatments can all improve the appearance of your skin and the acne. Do remember, however, that it’s important to get the acne under control first before tackling the scarring. Acne blue-light laser therapy programmes use intense blue wavelengths of light to destroy acne bacteria. Most people require six to eight treatments over a four-to-eight-week period for best results.
Why the ice cube method is getting so much buzz…
To shrink spots, try massaging them with an ice cube for around 15 seconds before bed. The ice will help shrink the inflammation.
Why it’s worth stocking up on the acne-fighting heroes…
Certain skincare ingredients can help keep post-pill acne under control and improve skin quality, and these are the best:
- Salicylic Acid – a pore detoxifying beta hydroxy acid that delves into your pores and unblocks them, reducing inflammation and controlling sebaceous gland activity.
- Hyaluronic Acid – hydrates, strengthens and replenishes the skin.
- Bentonite Clay – detoxifying, this ingredient draws out impurities from your pores for improved clarity.
- Kaolin Clay – drawing out impurities from within, this is an ingredient often found in clay-based face masks.
- Zinc & Sulphur – both of these are antimicrobial and anti-inflammatory minerals, so look out for them in SPF and other skincare products.
- Alpha Arbutin – this is best for inflammatory pigmentation control.
- Azelaic Acid & Retinoids – these are collagen-boosting ingredients designed to improve radiance and tackle scarring.
ADAPTING YOUR DAILY ROUTINE
Cleansing…
AM & PM – Use a gentle cleanser to keep your skin looking fresh and radiant. Avoid non-foaming cleansers as these can strip the skin of its essential oils, and use products that are non-comedogenic (non-pore clogging). As long as breakouts are severe, use ingredients like salicylic acid, lactic acid, or glycolic acid in a cream or gel formulation – both for your morning and evening cleanse.
Treating…
AM – You could try adding a prescriptive item into the mix here, such as Duac. This is a prescription-only product that contains benzoyl peroxide and clindamycin. This dream duo works together to soothe inflammation. You will need to see your doctor first, but I highly recommend it if your acne is acute. If your skin is prone to dryness, use a hydrating serum on top of the Duac. Look for serums full of nourishing and hydrating ingredients such as squalane, niacinamide and hyaluronic acid, and avoid oils – these can clog your pores and make your breakouts worse.
PM – Night is the best time to apply more powerful spot-busting actives that can get to work while you sleep. I normally add in a prescription strength of azelaic acid here (around 15-20%). This multitasking ingredient reduces inflammation, regulates oil control and also reduces pigmentation. Add retinoids for their collagen-building and acne-fighting properties. They also help to reduce pore inflammation, regulate sebaceous gland activity, speed up cell repair and treat post-inflammatory hyperpigmentation (dark spots).
Moisturising…
AM – Apply a protective hydrating and non-pore clogging moisturiser on top of your serum. This acts as a protective layer for your skin and locks in moisture, keeping the skin hydrated and the barrier strong.
PM – Often, the same moisturiser you use in the morning is adequate for acne sufferers, particularly if you’re using a good serum underneath. Again, avoid heavily oil-loaded products and look for natural emollients such as safflower, jojoba and squalane. I also love using peptides and hyaluronic acid in a night-time moisturiser.
For more information on Dr AJ Sturnham’s own skincare line, visit TheDecree.com.
SHOP OUR SKINCARE EDIT...
DISCLAIMER: We endeavour to always credit the correct original source of every image we use. If you think a credit may be incorrect, please contact us at info@sheerluxe.com.